Along with the changing colors on the trees, there is a chill in the air in metro Atlanta. Both are sure signs of fall! Another sign of the season can be found at any grocery or department store with pumpkins lining curbs out front and aisles of candy and costumes. Yet, even with the spooky delights of Halloween, a much more serious fright is observed during the third week of October with International Infection Prevention Week.
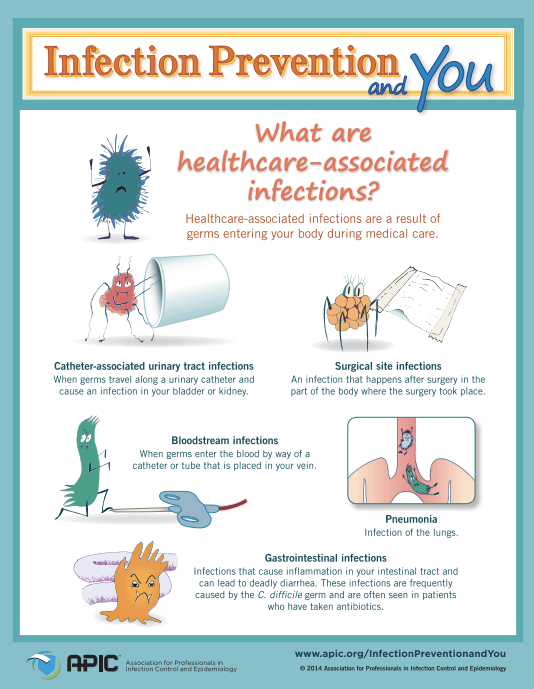
Image via APIC
This fright is a hidden one in the everyday world around us, and comes in the form of microbial organisms that cause infection, a major concern when it comes to disease control and prevention. While the healthcare industry is aware of the importance of washing hands, the message does not always get across to the general public or even within the healthcare industry itself. As reported in our Healthcare-Associated Infection information, more than 200 Americans are expected to pass away each day as a result of an infection contracted during a hospital stay.
Obviously, infections can be transmitted through other sources besides unwashed hands. However, this is one of the most basic places to start. For this reason, we support the Association for Professionals in Infection Control and Epidemiology (APIC) as they celebrate and promote awareness during International Infection Prevention Week. Here are a few tried and true pointers:
Infection Prevention at Work
No matter what industry you work in, whether it is healthcare, food preparation or service, education, government or private business, it is important to keep in mind general infection prevention practices. One way to prevent the spread of infection is through staying home from work or school when sick. This is not always practiced, but can easily make all a huge difference in the spread of diseases including common colds and the flu.
Infection Prevention at School
Parents of school-aged children know that colds and stomach bugs can pass through a classroom like wildfire. Encourage your child to make sure they are washing their hands regularly, especially after using the restroom and before eating. Another reminder for kids and adults includes sneezing or coughing into one’s elbow rather than into their hands.
Infection Prevention with Young Children
Young children may be at a higher risk for infection, but are also carriers of germs and bacteria especially on their hands. For this reason, it is important to instill proper handwashing procedures early on. One fun way to do this is to teach children to wash their hands while singing the entire ABC’s to make sure that they take enough time to lather up and scrub.
Lack of hand washing and other preventive measures likely contribute to the spread of infections. In cases involving healthcare facilities or professionals, sometimes infections may fall into the category of medical malpractice. In the state of Georgia, medical malpractice claims in are not easy to pursue, but the lawyers at Brownstein & Nguyen have years of experience successfully litigating cases like these. Contact our Atlanta malpractice attorneys for a free consultation if you or a loved one have suffered from a Healthcare-Associated Infection.